ACUTE & CHRONIC ANAL PAIN
- How do we assess and treat anal pain?
- How do we treat anal pain?
Before proceeding to any treatment in patient with acute and chronic anal pain is crucial to achieve the correct diagnosis and understand the true underlying reason which is responsible for this condition. Anal pain either acute or chronic may have different causes. In some circumstances patient present with pain as main symptom without any evidence of anal abnormalities. How do we establish the right diagnosis? The first step is obtaining complete past medical and surgical history and to understand if there is any trigger or predisposing factors that may have initiated the pain cycle. Some of the most important factors are:
- Acute constipation with excessive straining during defecation.
- History of chronic constipation with repeated excessive straining.
- History of single or multiples anal surgeries .
- History of single or multiple vaginal deliveries.
- History of prolonged labors or complicated vaginal deliveries.
- History of pelvic or sacral trauma.
It is also important to objectively assess the impact and relevance of that the pain and associated symptoms may have on the patient quality of life. For this purpose, we request the patient during or before the consultation to fill validated questionnaires which may help us to understand patient’s specific circumstances.
Physical examination including internal and the sternal assessment of the anal area is performed as initial step to understand and rule out the presence of any associated conditions that may be responsible for the patient’s symptoms. External examination would also include sensory blunt stimulations (Q-tip test) of the perianal and perineal area to map the pain territory distribution. Internal examination is performed whenever possible to establish is the compression of specific anatomical area triggers the onset of pain. Anoscopy is also performed to allow direct inspection of distal rectum and anal canal
The most common tests that are performed to investigate this condition are:
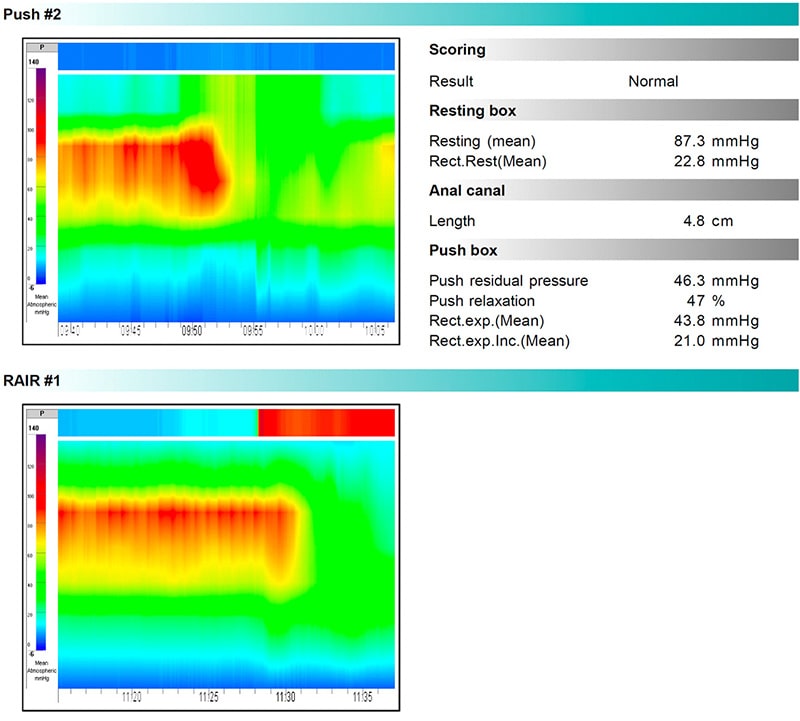
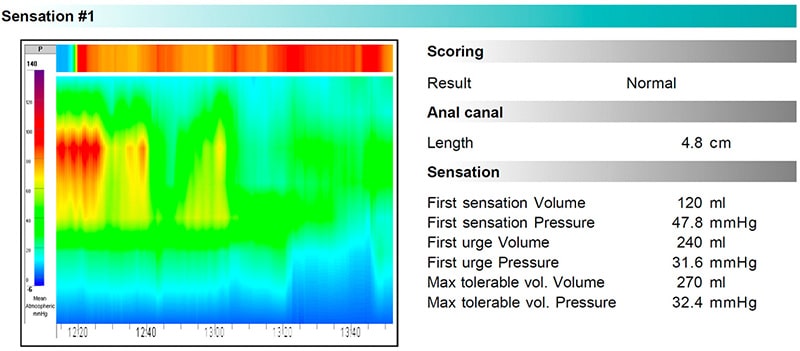
1.) High resolution Anorectal manometry which allow to define pressure of anal sphincter and distal rectum during resting, voluntary contraction and bearing down. This test is very detailed and is also able to identify incoordination of the anorectal segment during bearing down which may be the underlying cause of chronic anal pain in patients presenting with symptoms of excessive straining and difficult defecation. You can see how the test presents in its final lay out reporting different resting, working and sensory phases .


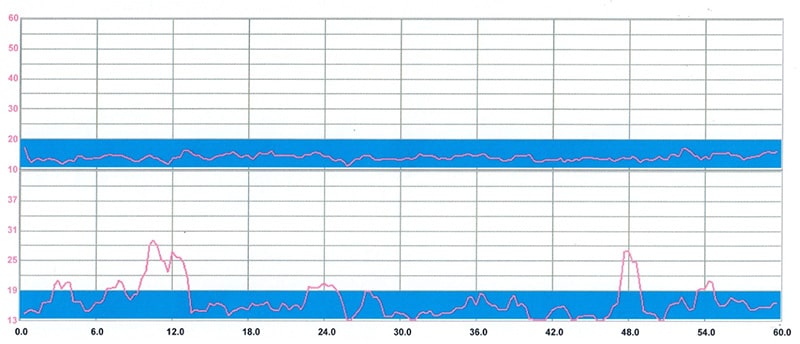
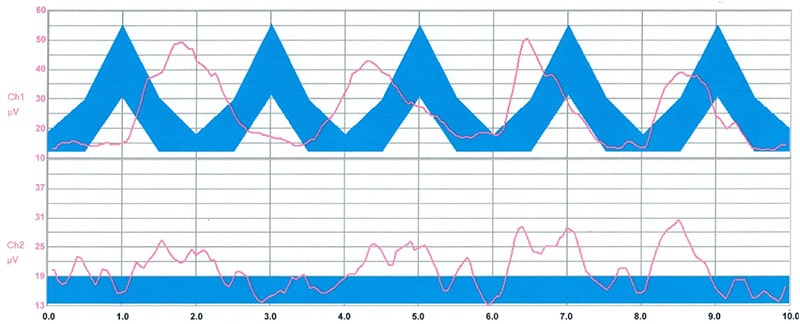
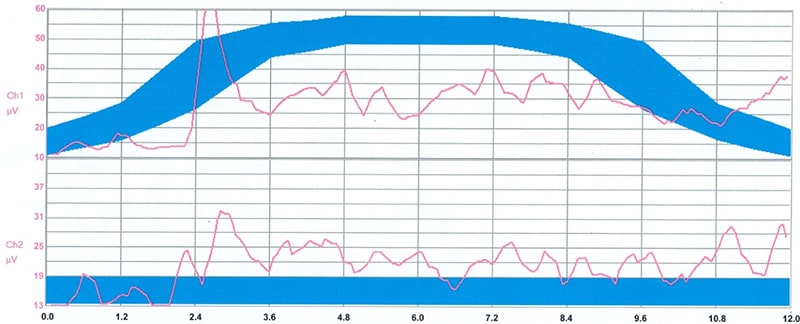
2.) Endo-anal and accessory muscle superficial electromyography assess anal sphincter muscle activity during resting and working phases such as squeezing and pushing and simultaneously record the activity of accessory muscles which may interfere negatively on the performance of the anal muscle activity. This test is also important to understand the level of control and command that the patient has on anal and pelvic muscles.
Resting
Rapid Squeeze Contraction
Endurance Squeeze Contraction
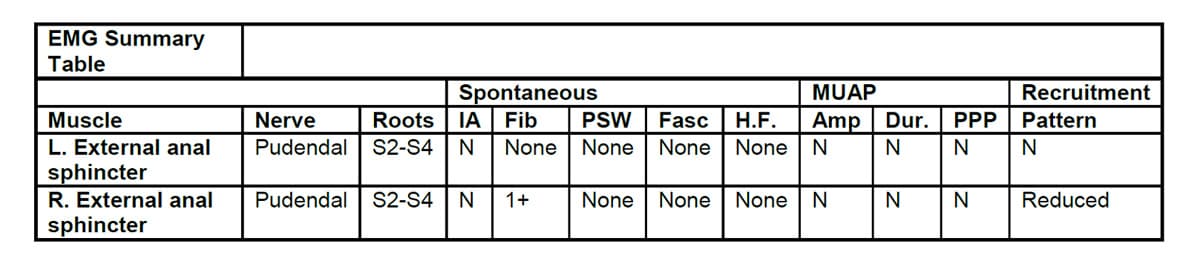
3.) Needle electromyography. This test is occasionally performed by our Consultant neurologist to assess if certain conditions such as post-traumatic denervation or paradoxical contraction of anal/pelvic muscle which may predispose to certain specific dysfunctions that interfere with normal rectal emptying during defecation leading to chronic excessive straining and ultimately to regional pain.
4.) Bulbo-Cavernous Muscle Nerve Latency Test. Some small electrical stimuli are delivered to genital area, and a computer will calculate the time needed for a reflex contraction of your anal sphincter. This assessment allows for determination of possible malfunction of the nerve.

5.) Sensory Evoked Potentials This study involves small electrodes being placed on the head, limbs and pelvic floor using small sticky electrodes and/or metal electrodes with a sticky paste. To test assess the integrity of nerve pathway.
Depending of the final diagnosis certain specific treatment are available to relieve the patient from pain and the most common are
1.) Chemodenervation of Internal Anal Sphincter with Botulin Toxin is performed in the early phases of anal pain when anal spasm is identified during Anorectal Manometry
2.) Pudendal Nerve anesthetic block under neurophysiological guidance is an office procedure done under local anesthesia where a needle connected to a special neuro-stimulating device allows the precise localization of the pudendal nerve followed by the injection of local anesthetic agent that blocks the sensory component of the nerve and therefore relief pain. This block as it temporary is also called test block but the duration and effect may be variable and in some patient its effect may be long-lasting. In the vast majority of patients, the effect only last for few days and then returns the usual levels. Despite that, a successful test block even for just few hours is a strong predictor of success another procedure we use to block the nerve for a longer period called Pulsed Radiofrequency.
3.) Pulsed radiofrequency is similar to the previous procedure as pudendal nerve is always reached via percutaneous injection under local anesthesia using the same neuro-stimulating device. When the nerve is reached a controlled thermal energy delivered by pulsed radiofrequency is applied to the nerve achieving a gentle heating, which ablate the sensory component of the nerve. The effect is long lasting usually from 4 to 24 months.
4.) Medical treatment is also utilized in addition or as substitute of nerve block in case of milder symptoms or contraindication to the above described procedure. Different medication effective on chronic pain may be used according to the doctor indications






